Here’s how
95% of organizations say their primary HR focus is their people’s health and wellbeing. We streamline your administration, so employees can get more from their benefits to make smarter decisions for their health. With our experience and expertise in employee benefits management, you can finally take care of your people and your spend.
Here’s the Challenge
Getting a handle on benefits is tough
Here’s how we solve it
Unlock true engagement
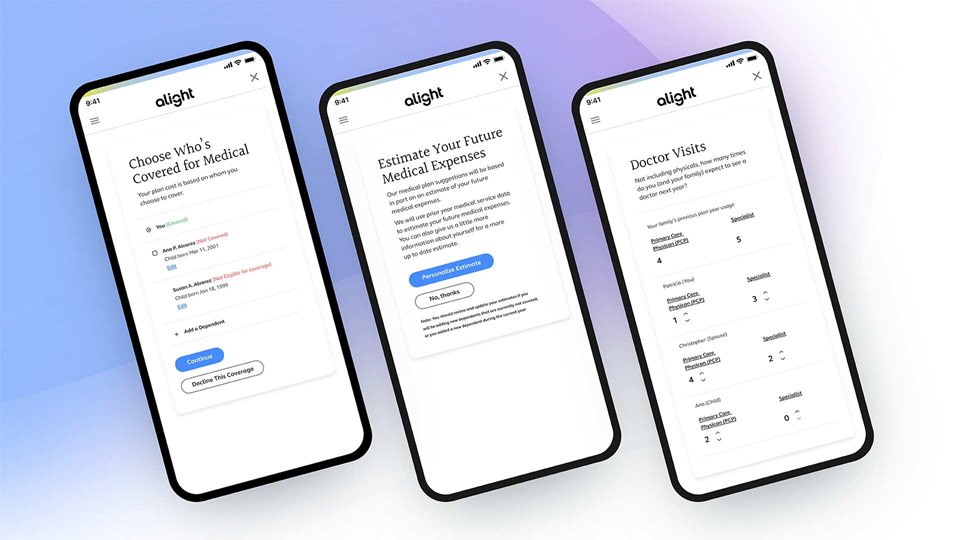
1:1 benefits open enrollment
1,000 or 100,000 employees, it doesn’t matter. Each one gets a tailored enrollment experience with a few questions to kick it off and personalized suggestions that follow, all backed by extensive data.

A closer look at engagement
By personalizing the experience and giving employees the tools to make smart moves, we can check off your benefit admin goals together.
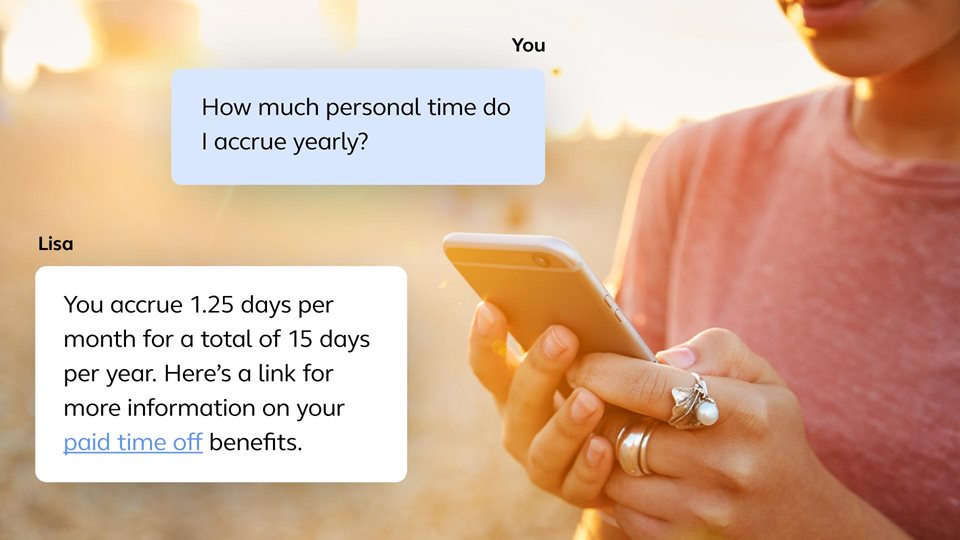
Work smarter in one spot
From web to mobile to the intelligent virtual assistant, meet your people where they are with an omni-channel experience — enabling smarter work and life decisions for your people and actionable insights for you.
More of what’s possible with Benefits Administration
For employers
When it comes to employee benefits management, we’ve really seen it all. We support over 13,000 different health plan designs, with 12 million people using our platform. By continuously analyzing employee behavior, we connect them to your programs more reliably while ensuring you both save.
Benefits
- Specifically designed to meet your benefits strategy
- Easily and effectively enroll new employees
- Help your people make smart decisions throughout the year
- Easy and intuitive to administer your benefits program as an employer
- Provide a global digital solution to connect employees worldwide with expertise at the local level

For employees
Choosing benefits shouldn’t be complicated. Our full range of intuitive plan solutions guide employees to clear health and wellbeing choices, from their first day to retirement.
Benefits
- Take control of health with simplified offering and decision making
- Experience personalized interactions that drive benefits satisfaction

Frequently asked questions
Have a particular question about employee benefits management? We've answered some of the most commonly asked questions.
What is benefits administration?
Benefits administration involves designing and managing employee benefits programs within a company. Successful benefits administration process strikes a balance between offering a positive employee experience and ensuring business efficiency and compliance. More details at Ask Alight: What is benefits administration?
What does it mean to outsource your benefits administration?
When a company decides to outsource its benefits administration, it partners with an outside company to take on specific responsibilities related to administering benefits to its employees. Learn more at Ask Alight: What is benefits administration?
Customer story
Ready to get started?
Learn more about how we can help your business.
Recommended insights
Explore our other solutions
Alight Total Health
A comprehensive health benefits solution with guaranteed ROI.
Healthcare Navigation
Guide your people to the right care and savings from the start.
Reimbursement Accounts
Strategic reimbursement accounts for your people to save and feel secure.
Dependent Eligibility & Compliance
Stay on top of regulations and avoidable expenses, even as things change.




