Here’s how
95% of organizations say their primary HR focus is their people’s health and wellbeing. We streamline your administration, so employees can get more from their benefits to make smarter decisions for their health. With our experience and expertise, you can finally take care of your people and your spend.
Here’s the Challenge
Getting a handle on benefits is tough
Here’s how we solve it
Unlock true engagement
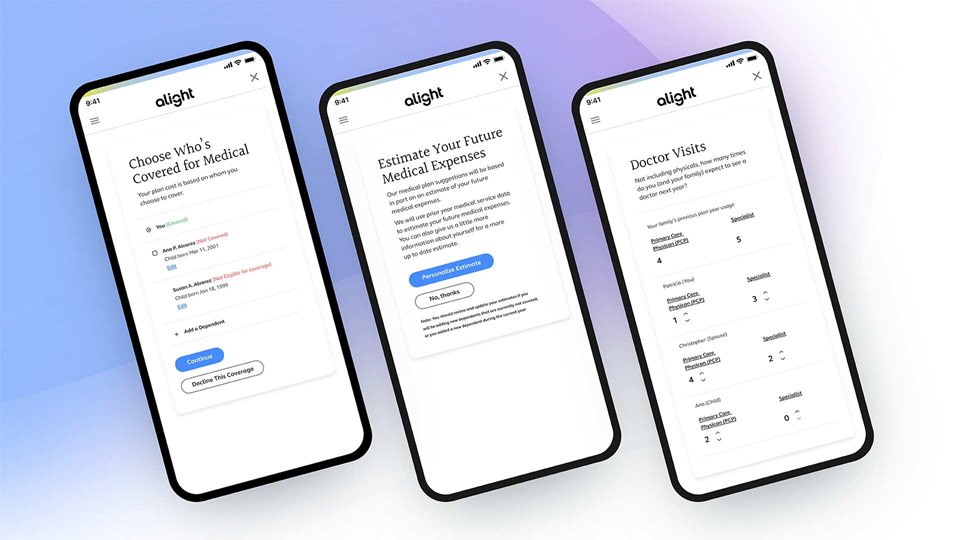
1:1 benefits open enrollment
1,000 or 100,000 employees, it doesn’t matter. Each one gets a tailored enrollment experience with a few questions to kick it off and personalized suggestions that follow, all backed by extensive data.

A closer look at engagement
By personalizing the experience and giving employees the tools to make smart moves, we can check off your benefit admin goals together.
Work smarter in one spot
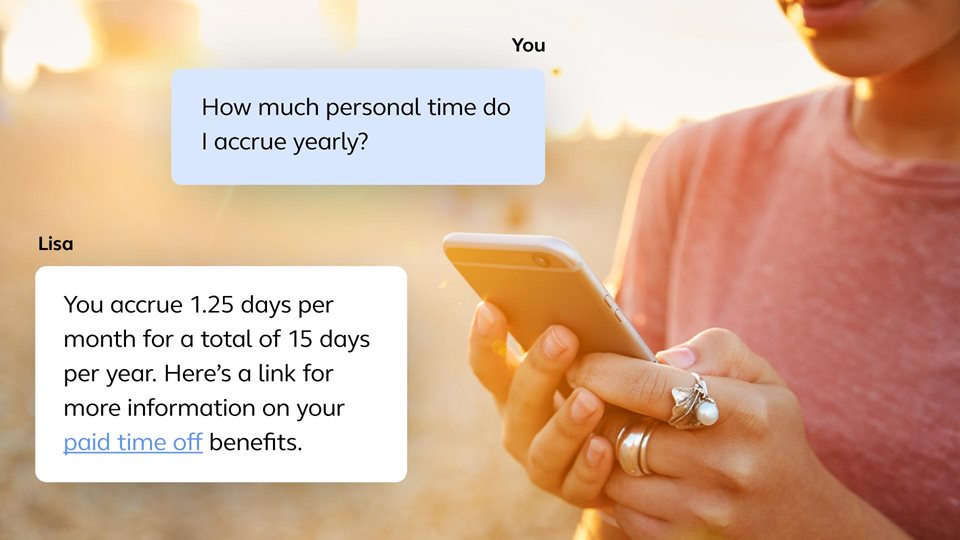
From web to mobile to the Ask Lisa chatbot, meet your people where they are with an omni-channel experience — enabling smarter work and life decisions for your people and actionable insights for you.
More of what’s possible with Benefits Administration
For employers
When it comes to benefits, we’ve really seen it all. We support over 13,000 different health plan designs, with 12 million people using our platform. By continuously analyzing employee behavior, we connect them to your programs more reliably while ensuring you both save.
Benefits
- Specifically designed to meet your benefits strategy
- Easily and effectively enroll new employees
- Help your people make smart decisions throughout the year
- Easy and intuitive to administer as an employer
- Provide a global digital solution to connect employees worldwide with expertise at the local level

For employees
Choosing benefits shouldn’t be complicated. Our full range of intuitive plan solutions guide employees to clear health and wellbeing choices, from their first day to retirement.
Benefits
- Take control of health with simplified offering and decision making
- Experience personalized interactions that drive benefits satisfaction

Frequently asked questions
Have a particular question about Health Benefits Administration? We've answered some of the most commonly asked questions.
What is health benefits administration?
Health benefits administration has two major functions. First, open enrollment (or new hire enrollment) is when your employees sign up for their health care benefits. Second, ongoing support is provided to answer questions and provide your people with education and guidance throughout the year. While enrollment may be the most well-known part of health benefits administration, Alight believes ongoing support is the key to a successful outsourcing partnership.
What does it mean to outsource your benefits administration?
When a company decides to outsource its benefits administration, it partners with an outside company to take on specific responsibilities related to administering health benefits to its employees.
Why outsource your benefits administration?
Outsourcing liberates internal resources from transactional activities related to benefits, including open enrollment, verifying dependents, processing life event changes and answering health benefits and other questions. Having an outside expert administer your benefits reduces the expenses associated with manual errors and premium overpayments.
How does outsourcing benefits save my organization money?
In addition to freeing up your internal resources and time, you can save money automating data and event processing, which is embedded into Alight’s benefit administration solutions. This process generates savings through timely terminations (both employee and ineligible dependents), accurate payroll deductions and frequent carrier updates.
What are the steps in implementing a health benefits administration program?
(1) Determine benefits eligibility – including dependent verification. (2) Provide health benefits information – both online and offline. (3) Make sure to provide any legally required disclosures or notices. (4) Enroll employees and their families for their selected benefits.
How do I ensure my plans are compliant with the ACA (Affordable Care Act)?
Alight eliminates the risk of self-administering or using multiple vendors. Our compliance services include ongoing monitoring to mitigate risk and developing solutions to support your compliance with regulations, including the ACA. Alight continually stays on top of new laws and regulations, and then updates our solutions and processes as required to support your compliance.
Customer story
Ready to get started?
Learn more about how we can help your business.
Recommended insights
Explore our other solutions
Alight Total Health
A comprehensive health benefits solution with guaranteed ROI.
Healthcare Navigation
Guide your people to the right care and savings from the start.
Reimbursement Accounts
Strategic reimbursement accounts for your people to save and feel secure.
Dependent Eligibility & Compliance
Stay on top of regulations and avoidable expenses, even as things change.




