Essilor of America, a leading provider of eyeglass lenses, was seeking a solution to achieve two of its organizational healthcare objectives—lowering its healthcare cost trajectory and improving participant decision making. With an average employee age of 47 years-old and a workforce of 8,500 spread over 120 locations across the U.S., Essilor needed a solution to assist employees with navigating their healthcare benefits by choosing the right providers from the start.

Transform your healthcare spend — How Essilor of America achieved 2.7x ROI
Many organizations are facing the challenge of rising healthcare costs. How are you managing this for your organization? Are you proactive or reactive?
The problem: a reactive approach to controlling healthcare costs
Like most organizations, Essilor historically had a reactive approach to controlling healthcare costs. Meaning, Essilor controlled organizational healthcare costs year over year by shifting more and more of the cost to employees. The problem with this reactive approach is that organizations can only do this for so long before they start to jeopardize the competitiveness of their benefits offering in the market.
Essilor was starting to reach that point—they had very little runway left in terms of increasing plan deductibles in order to lower the company-paid portion of the premium. With an aging workforce, they knew they needed to do something different and be more proactive with engaging employees in making better healthcare decisions.
About Essilor of America
- 8,500 employees
- 150 locations across the U.S.
- Average age: 47 years old
- 2/3 employees work in production labs
- 1/3 have admin jobs
In 2016, Essilor partnered with Alight’s Healthcare Navigation Solution to help employees maximize benefits, improve outcomes and lower overall health plan costs. Accessible via phone, email, web or mobile app, their Alight Health Pro®, Kaylie, acts as an employee’s personal healthcare concierge, providing high-touch, white-glove assistance with virtually all aspects of the healthcare experience, including:
- High-quality, cost-effective doctor and care recommendations
- Verification of coverage
- Cost estimates
- Appointment scheduling
- Prescription reviews
- Bill reviews
- Medical record transfers
- Coordination of care
They initially rolled out the solution to only a portion of the workforce, focusing on a smaller subsection of employees to more easily integrate the tool and gain user buy-in. As utilization rates steadily increased, Essilor decided to expand the tool to the entire employee population, making it easier for the team to release broad communications and information.
With an aging workforce, we knew we had to be proactive, specifically with offering different clinically proven programs to help improve the overall health of the Essilor population...Alight has been a really great partner with integrating different clinical programs into the population and reinforcing the programs. It really is the single source where employees can go to get all their questions answered about their healthcare.
Essilor of America
Establish healthcare navigation as the front door of the plan
Essilor positioned Alight as the front door to its health plan so employees could make more proactive healthcare decisions. Most organizations underestimate the costs associated with employees going to the wrong doctor. Research suggests that when people find doctors through mediums like Google, Yelp and friends/family, they find doctors below the 50th percentile who are associated with lower quality, expensive care. Essilor knew they needed to get employees to the right providers from the start.
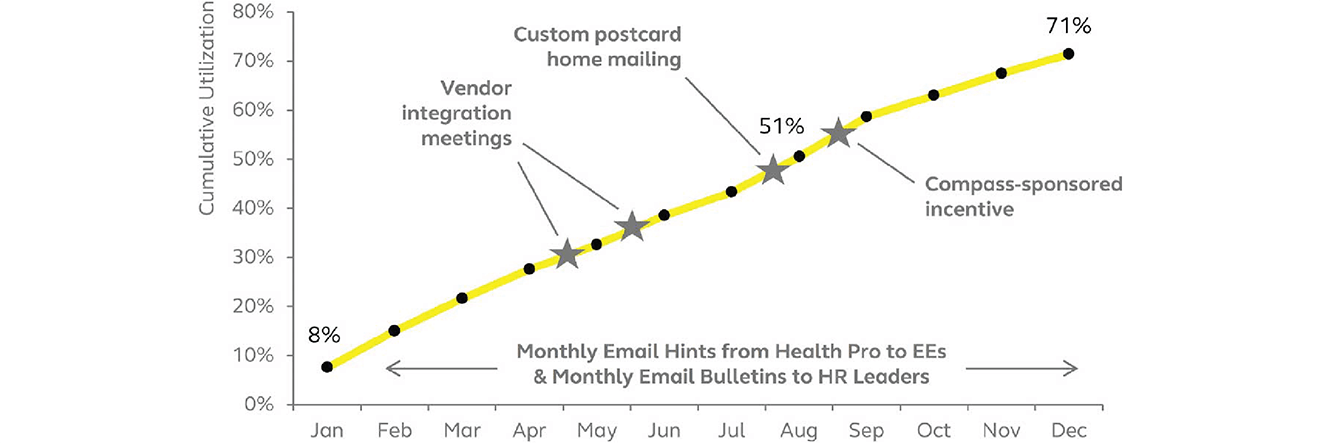
From 2016 to 2018, they released a constant flow of information and communications going out to employees, but because of the employee demographic, the team realized that not everyone paid attention to email. Consequently, they developed creative means to reach employees and drive engagement, such as postcards with snapshots of relevant information. They also held different events throughout the year to promote participation, like hosting vendor integrations meetings.
Essilor made sure that employees could access the service in the most efficient ways possible, whether it be from a web-based platform or on a mobile device. They also ensured that all communications came directly from Kaylie, their Health Pro© consultant, to make it easier to instantly reply or to dive right into the service for more detailed assistance or information.
With Alight as the front door to their health plan, Essilor maintained a consistent employee interface which enabled them to evolve their benefits strategy over time to meet the needs of their people. As Essilor slowly reached its goal of increasing participant participation, it focused on smaller goals as well, such as making sure employees received—at a minimum—an annual physical exam with a primary care doctor.
Helping people make smarter choices throughout the year
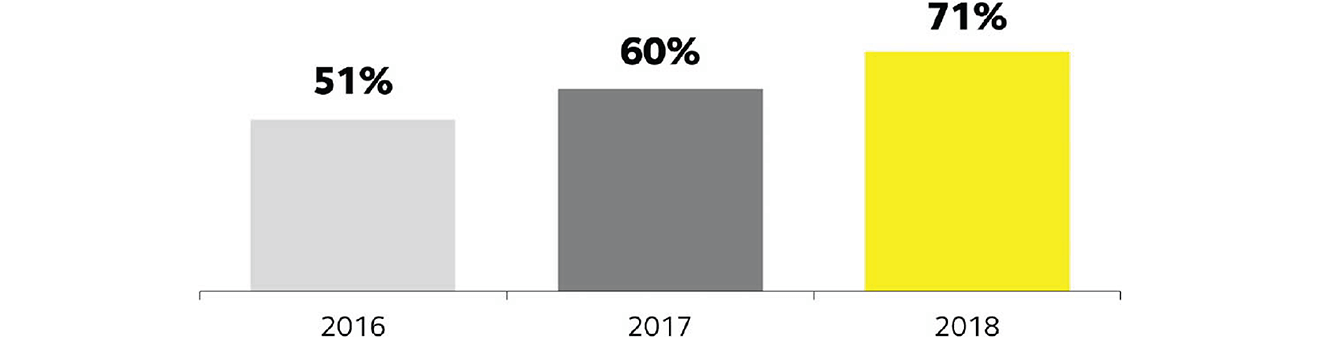
Looking back on data from 2016 to 2018, Essilor saw a steady increase in utilization year over year. In 2016, they provided almost 800 healthcare navigation solutions for employees. Meaning, their Alight Health Pro© consultant was engaged 800 times that year and provided a solution to a problem or an answer to a healthcare related question. This number increased steadily over the years as utilization rates increased. As of 2019, Essilor has rolled out the Alight Healthcare Navigation Solutions program to its entire employee population; they are on trend to have around 1,900 solutions by year-end. As more solutions are being offered and utilized by employees, it translates to more employees getting the right information to make better decisions about healthcare.
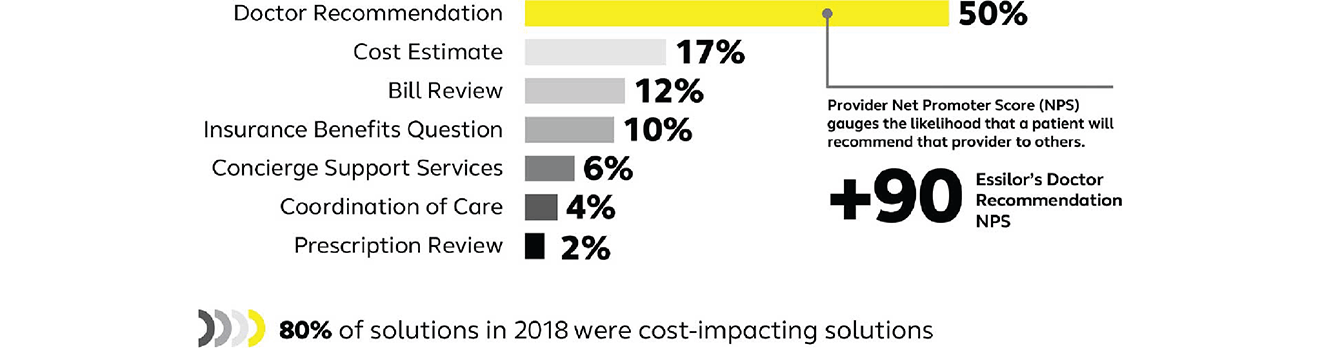
How Essilor employees use Alight
The #1 way Essilor participants use Alight is to get to the right provider from the start. When people “walk through the wrong provider’s door” there is a snowball effect that costs the participant and Essilor unnecessary money.
2018 Cumulative utilization by month
Growing employee engagement year-over-year
Results
Not only did Essilor accomplish its goal of helping participants make smarter healthcare decisions and getting people to the right doctor from the start, the organization also experienced significant impacts on its healthcare costs and overall ROI.
2018 results
User stats
User satisfaction — Net Promoter Score (NPS)
Looking forward
Ryan Murry, Essilor’s Director of Compensation and Benefits, offers HR peers his most valuable tips when it comes to implementing a healthcare navigation solution.
- Effectively communicate—Essilor recognized that utilization would only be successful if employees were aware and informed. Constant, tailored communications that meet people where they are ensure employees are being reached in most effective way. This allows them to best understand and take advantage of relevant programs and services.
- Recognize that adoption doesn’t happen overnight—Successfully transitioning to a healthcare navigation tool isn’t instantaneous. Putting in the effort and partnering with a flexible solution, such as Alight Navigator, and other vendors provide convenient, assorted solutions to employees. Implementation should be a focused effort with clear goals.
- Get people to the right providers from the start—To improve the health of your people and control plan costs, you must get people to engage at the right point in time with the right provider—a provider that will not only deliver a great care experience, but also likely lower costs for your people and the plan.
Why Alight?
Do more with a single platform. Drive benefits strategy, not just benefits administration
Essilor’s concern about a reactive approach to controlling healthcare costs is not an uncommon fear; many organizations are experiencing similar situations with their own employees and healthcare products. By partnering with Alight’s Healthcare Navigation Solution, Essilor achieved 2.7x ROI in 2018—$185k in claims verified savings—and a 71% utilization rate. Helping participants get to the right provider from the start and make smarter, more cost-effective healthcare decisions enabled Essilor to lower healthcare costs and increase participant satisfaction.
Alight’s Healthcare Navigation Solutions deliver far more than mere cost savings. They empower employees and their families to:
- Make informed healthcare decisions
- Identify highly-rated, cost-effective providers
- Know the cost of care in advance
- Overcome the inevitable healthcare hassles like verifying coverage, scheduling appointments for preventive and routine care, procedures and surgeries and resolving billing questions and disputes
Let's talk
Interested in Alight’s Healthcare Navigation Solutions but not sure where to start? We can help.


